داء العطائف
| Campylobacter | |
|---|---|
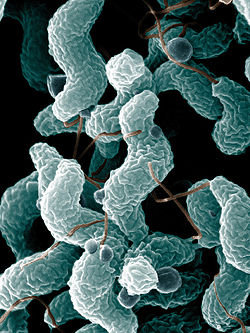 | |
| البكتربا الكامبيلوباكتيرية هى السبب رقم-1 للداء المرتبط بالغذاء المعدى-معوى في الولايات المتحدة. هذه الصورة بالميكروسكوب الإليكترونى تظهر الشكل المميز الحلزونى او المنحنى, أو مثل سدادة الفلين C. jejuni خلايا وما بشبهها . | |
| التبويب والمصادر الخارجية | |
| التخصص | الأمراض المعدية (تخصص طبي) |
| ICD-10 | A04.5 |
| ICD-9-CM | 008.43 |
| DiseasesDB | 1914 |
| MedlinePlus | 000224 |
| eMedicine | ped/2697 med/263 |
| Patient UK | فشل عرض الخاصية P1461: لم يتم العثور على الخاصية P1461. داء العطائف |
| MeSH | D002169 |
Campylobacteriosis عدوى الكامبايلوباكتريا هى عدوى بكتيرية تتم بواسطة campylobacter bacterium [1], most commonly C. jejuni. وهى تعد من أكثر أنواع العدوى شيوعا العدوى البكتيرية للإنسان [[ غالبا عدوى التسمم الغذائى. تنتج إلتهابى , أو دموي , إسهال أو زحار متلازمة, وتشمل في الغالب تقلصات , حمي و ألم .
الأسباب
Campylobacteriosis تسببهاCampylobacter مبكروبات. منحنية أو حلزونية, متحركة, لاتكون حويصلات, سالبة الجرام عصيات . و في الغالب مصدرها C. jejuni, بكتيريا حلزونية و منحنية الشكل توجد في الماشية غالبا , الخنازير , والطيور ولكنها غير معدية . و يمكن أن يتسبب المرض بواسطة C. coli (يوجد أيضا في الماشية, و الخنازير والطيور) C. upsaliensis (يوجد في القطط , والكلاب) و C. lari (يوجد في الطيور البحرية على وجه الخصوص).
أهم سبب للعدوى بالمرض campylobacteriosis الكامبيلوباكتيرية الإصابة بجرح في النسيج الداخلى المعدة. أماكن الجرح الداخلى jejunum, الدقاق, و colon. C jejuni يبدو أن ذلك يسببه تدمير الخلايا الطلائية المبطنة لجدار المعدة الذى تسببه البكتيربا الكامبيلوباكتيرية.
بعض فصائل C jejuni تنتج سم داخلى شبيه بمثيله في كوليرا, الذى يعول عليه في الإسهال المائى الملاحظ في تلك العدوات. و تنتج البكتيريا إفراز منتشر دموىمتقيح , إلتهاب داخلى. في عدد قليل من الحالات , و تقترن العدوى hemolytic uremic syndrome و thrombotic thrombocytopenic purpura من خلال آلية عمل , غير مفهومة .
إنتقال العدوى
The common routes of transmission for the disease-causing bacteria are fecal-oral, person-to-person sexual contact, ingestion of contaminated food (generally unpasteurized (raw) milk and undercooked or poorly handled poultry), and waterborne (ie, through contaminated drinking water). Contact with contaminated poultry, livestock, or household pets, especially puppies, can also cause disease.[2] Animals farmed for meat are the main source of campylobacteriosis. A study published in PLoS Genetics (September 26, 2008) by researchers from Lancashire, England, and Chicago, IL, found that 97 percent of campylobacteriosis cases sampled in Lancashire were caused by bacteria typically found in chicken and livestock. In 57 percent of cases, the bacteria could be traced to chicken, and in 35 percent to cattle. Wild animal and environmental sources were accountable for just three percent of disease.[3]
The infectious dose is 1000-10,000 bacteria (although ten to five hundred bacteria can be enough to infect humans). Campylobacter species are sensitive to hydrochloric acid in the stomach, and acid reduction treatment can reduce the amount of inoculum needed to cause disease.
Exposure to bacteria is often more common during travelling, and therefore campylobacteriosis is a common form of travelers' diarrhea.
علم الأويئة
Infection with a Campylobacter species is one of the most common causes of human bacterial gastroenteritis.[4] For instance, an estimated 2 million cases of Campylobacter enteritis occur annually in the U.S., accounting for 5-7% of cases of gastroenteritis. Furthermore, in the المملكة المتحدة during 2000 campylobacter jejuni was involved in 77.3% in all cases of foodborne illness[5]. 15 out of every 100,000 people are diagnosed with campylobacteriosis every year, and with many cases going unreported, up to 0.5% of the general population may unknowingly harbor Campylobacter in their gut annually.
A large animal reservoir is present as well, with up to 100% of poultry, including chickens, turkeys, and waterfowl, having asymptomatic infections in their intestinal tracts. An infected chicken may contain up to 109 bacteria per 25 grams, and due to the installations, the bacteria is rapidly spread to other chicken. This vastly exceeds the infectious dose of 1000-10,000 bacteria for humans.
الأعراض
The prodrome is fever, headache, and myalgias, lasting as long as 24 hours. The actual latent period is 2-5 days (sometimes 1-6 days). In other words, it typically takes 1-2 days until actual symptoms develop.[مطلوب توضيح] These are diarrhea (as many as 10 watery, frequently bloody, bowel movements per day) or dysentery, cramps, abdominal pain, and fever as high as 40°C. In most people, the illness lasts for 2–10 days.
Symptoms may also depend on route of transmission. In participants of anoreceptive intercourse, campylobacteriosis is more localized to the distal end of the colon and may be termed a proctocolitis.
There are other diseases showing similar symptoms. For instance, abdominal pain and tenderness may be very localized, mimicking acute appendicitis. Furthermore, Helicobacter pylori is closely related to Campylobacter and causes peptic ulcer disease.
العوامل الأخرى
In patients with HIV, infections may be more frequent, may cause prolonged of dirty brown diarrhea, and may be more commonly associated with bacteremia and antibiotic resistance. The severity and persistence of infection in patients with AIDS and hypogammaglobulinemia indicates that both cell-mediated and humoral immunity are important in preventing and terminating infection.
التشخيص
Campylobacter organisms can be detected on gram stain of stool with high specificity and a sensitivity of ~60%, but are most often diagnosed by stool culture. Fecal leukocytes are present and indicate an inflammatory diarrhea.
العلاج
The infection is usually self-limiting and in most cases, symptomatic treatment by reposition of liquid and electrolyte replacement is enough in human infections.[6] The use of antibiotics is controversial.
Antimotility agents, such as loperamide, can lead to prolonged illness or intestinal perforation in any invasive diarrhea, and should be avoided.
المضادات الحيوية
Antibiotic treatment has only a marginal benefit (1.32 days) on the duration of symptoms and should not be used routinely.[7]
Erythromycin can be used in children, and tetracycline in adults. However, some studies show that erythromycin rapidly eliminates Campylobacter from the stool without affecting the duration of illness. Nevertheless, children with dysentery due to C. jejuni benefit from early treatment with erythromycin. Treatment with antibiotics, therefore, depends on the severity of symptoms. Quinolones are effective if the organism is sensitive, but high rates of quinolone use in livestock means that quinolones are now largely ineffective.[8]
Trimethoprim-sulfamethoxazole and ampicillin are ineffective against Campylobacter.
في الحيوانات
In the past, poultry infections were often treated by mass administration of enrofloxacin and sarafloxacin for single instances of infection. The FDA banned this practice, as it, instead of eliminating the bacteria, only promoted the development of fluoroquinolone-resistant populations. [9] A major wide-ranged fluoroquinolone used in humans is ciprofloxacin.
تطور المرض
Campylobacteriosis is usually self-limited without any mortality. However, there are several possible complications.
المضاعفات
Some (less than 1 in 1000 cases) individuals develop Guillain-Barré syndrome, in which the nerves that join the spinal cord and brain to the rest of the body are damaged, sometimes permanently. This occurs only with infection of C. jejuni and C. upsaliensis. [10]
Other complications include toxic megacolon, dehydration and sepsis. Such complications generally form in little children ( < 1 year of age) and immunocompromised people. Chronic course of the disease is possible; such form of the process is likely to develop without a distinct acute phase. Chronic campylobacteriosis features long period of sub-febrile temperature and asthenia; eye damage, arthritis, endocarditis may develop if infection is untreated.
Occasional deaths occur in young, previously healthy individuals because of volume depletion and in persons who are elderly or immunocompromised.
A mysterious paralysis can attack people who just had mild symptoms of campylobacteriosis years earlier.[11]
الوقاية أو منع العدوى
- Pasteurization of milk and chlorination of drinking water destroy the organism.
- Treatment with antibiotics can reduce fecal excretion.
- Infected health care workers should not provide direct patient care
- Separate cutting boards should be used for foods of animal origin and other foods. After preparing raw food of animal origin, all cutting boards and countertops should be carefully cleaned with soap and hot water.
أنظر أيضا
المراجع
- ^ cdc.gov
- ^ Saenz Y, Zarazaga M, Lantero M, Gastanares MJ, Baquero F, Torres C (2000). "Antibiotic resistance in Campylobacter strains isolated from animals, foods, and humans in Spain in 1997-1998". Antimicrob Agents Chemother. 44 (2): 267–71. doi:10.1128/AAC.44.2.267-271.2000. PMID [http://aac.asm.org/cgi/content/full/44/2/267 fulltext 10639348 [http://aac.asm.org/cgi/content/full/44/2/267 fulltext]].
{{cite journal}}: Check|pmid=value (help); External link in|pmid= - ^ Animals Farmed for Meat Are the Number 1 Source of Food Poisoning Bug Newswise, Retrieved on September 23, 2008.
- ^ Moore, 2005
- ^ Food Standards Agency
- ^ Sherris
- ^ Ternhag A, Asikainen T, Giesecke J, Ekdahl K (2007). "A meta-analysis on the effects of antibiotic treatment on duration of symptoms caused by infection with Campylobacter species". Clin Infect Dis. 44: 696–700. doi:10.1086/509924.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Fàbrega A, Sánchez-Céspedes J, Soto S, Vila J (2008). "Quinolone resistance in the food chain". Int J Antimicrob Agents. 31 (4): 307–15. doi:10.1016/j.ijantimicag.2007.12.010. PMID 18308515.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ McDermott P, Bodeis S, English L, White D, Walker R, Zhao S, Simjee S, Wagner D (2002). "Ciprofloxacin resistance in Campylobacter jejuni evolves rapidly in chickens treated with fluoroquinolones". J Infect Dis. 185 (6): 837–40. doi:10.1086/339195. PMID 11920303.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Medical microbiology,Murray, P.R. and others. 2002 Mosby St. Louis
- ^ Food poisoning can be long-term problem by Lauran Neergaard, accessed 21 January 2008