تسمم سجقي
| Botulism | |
|---|---|
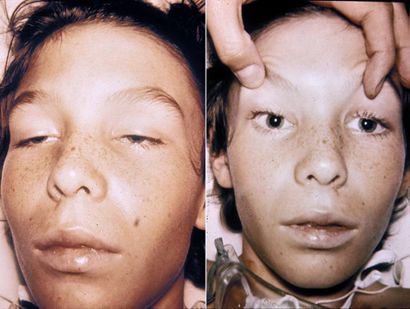 | |
| A 14-year-old with botulism, characterised by weakness of the eye muscles and the drooping eyelids shown in the left image, and dilated and non-moving pupils shown in the right image. This youth was fully conscious. | |
| النطق | |
| التخصص | Infectious disease, gastroenterology |
| الأعراض | Weakness, trouble seeing, feeling tired, trouble speaking[1] |
| المضاعفات | Respiratory failure[2] |
| البداية المعتادة | 12 to 72 hours[2] |
| المدة | Variable[2] |
| المسببات | Clostridium botulinum[1] |
| الطريقة التشخيصية | Finding the bacteria or their toxin[1] |
| التشخيص المفاضل | Myasthenia gravis, Guillain–Barré syndrome, Amyotrophic lateral sclerosis, Lambert Eaton syndrome[3] |
| الوقاية | Proper food preparation, no honey for children less than one[1] |
| العلاج | Antitoxin, antibiotics, mechanical ventilation[1] |
| Prognosis | ~7.5% risk of death[1] |
Botulism (Latin, botulus, "sausage") يعرف أيضا ب"Botulinus التسمم," نادر ولكن شديد الخطورة paralytic illness caused by botulin toxin. التوكسين ينتج بواسطة البكتيريا Clostridium botulinum. C. botulinum يكونanaerobic, موجبة الجرام, عصيات مكونة للكبسولات(Spores ).وتوكسين البوتيولين أشدالتوكسينات فعالية وخطورة إن واحد ميكروجرام يعد قاتلا للإنسان,وهو يعمل بإغلاق وظائف العصب حيث يؤدى respiratory و musculoskeletal paralysis.
توجد ثلاثة أنواع من Botulism توكسين :
- Infant botulism أو botulism المعوى يسببه إبتلاع كبسولات(Spores ) spores الC. botulinum, التى تنمو حينئذ داخل معى الطفلintestines و يتم تحرر التوكسين .
- Foodborne botulism يتم بتناول المأكولات التى تحوى botulin توكسين .
- Wound botulism, الأقل شيوعا بين الثلاثة, يسببه botulin توكسين الذى ينتج داخل الجرحالمصاب ب C. botulinum.
كل صور البوتيولين قاتلة ,و تعد دائما من الطوارىء الطبية. Foodborne botulism يمكن أن يعد خطرا للغاية كpublic health خطورة لأن أشخاصا عديدين يمكن أن يستهلكوا المادة السامة من مصدر غذائى واحد ملوث .
الإنتشار
An average of 110 cases of botulism are reported each year in the الولايات المتحدة. Of these, approximately, 72% are infant botulism, and 3% are wound botulism. Outbreaks of foodborne botulism involving two or more persons occur during most years and are usually caused by the consumption of home-canned foods. The number of cases of foodborne and infant botulism has changed little in recent years, but wound botulism has increased because of the use of black tar heroin, especially in كاليفورنيا.[4] In July 2007, a widespread recall was initiated due to botulism contamination of food manufactured by Castleberry's Food Company.[5] Shortly thereafter, in August 2007, the FDA issued a warning of botulism risk from canned French cut green beans manufactured by Lakeside Foods Inc, of Manitowoc, Wisconsin.[6]
الأعراض
البوتيوليزم التي تنقلها الأغذية وجروح التسمم
- Normal symptoms of food-borne botulism usually occur between 12–38 hours after consuming the botulinum toxin. However, they can occur as early as 6 hours or as late as 10 days after.
- Wound botulism has a longer incubation period, usually between 4–14 days.
Normal symptoms include dry mouth, double and/or blurred vision, difficulty swallowing, muscle weakness, drooping eyelids, difficult breathing, slurred speech, vomiting, urinary incontinence and sometimes diarrhoea. These symptoms may continue to cause paralytic ileus with severe constipation, and will lead to body paralysis. The respiratory muscles are affected as well, which may cause death due to respiratory failure. These are all symptoms of the muscle paralysis caused by the bacterial toxin.
In all cases illness is caused by the toxin made by C. botulinum, not by the bacterium itself. The pattern of damage occurs because the toxin affects nerves that are firing more often.[7] Specifically, the inhibition of the release of Acetylcholine from motor neurons, which synapse with the myofibers at the neuro muscular junction, results in a loss of muscle function, and paralysis.
دراسة حالة
On July 2, 1971, FDA released a public warning after learning that a New York man had died and his wife had become seriously ill due to botulism after eating a can of Bon Vivant vichyssoise soup.The diagnosis was made by Dr. Henry P. Colmore in Mt. Kisco, New York. The company commenced a recall of the 6,444 cans of vichyssoise soup from the same batch. An effectiveness check of the recall revealed a number of swollen or otherwise suspect cans among Bon Vivant's other products, leading the FDA to question Bon Vivant's processing practices for all products. Five cans of soup were found to be contaminated with the botulin toxin, all from the batch initially recalled, and the FDA extended the recall to include all Bon Vivant products, and shut down the company’s Newark, New Jersey, plant on 7 July, 1971.
بوتيوليزم الرضع
Infant botulism (first recognized in 1976) is the most common form of the ailment in the United States. It affects about 100 infants per year in the United States. Infants less than 12 months of age are susceptible, with almost 90% of cases occurring between the ages of 3 weeks and 6 months of age at presentation. The mode of action of this form is through colonization by germinating spores in the gut of an infant. The first symptom is usually constipation, followed by generalized weakness, loss of head control and difficulty feeding. Like the other forms of botulism, the symptoms are caused by the absorption of botulinum toxin, and typically progress to a symmetric descending flaccid paralysis. Death is often the eventual outcome unless the infant receives artificial ventilation. Infants under the age of 1 should not have corn syrup or honey.
Honey, corn syrup, and other sweeteners are potentially dangerous for infants. This is partly because the digestive juices of an infant are less acidic than older children and adults, and may be less likely to destroy ingested spores. In addition, young infants do not yet have sufficient numbers of resident microflora in their intestines to competitively exclude C. botulinum. Unopposed in the small intestine, the warm body temperature creates a medium for botulinum spores to germinate, divide and produce toxin. Thus, C. botulinum is able to colonize the gut of an infant with relative ease, whereas older children and adults are not typically susceptible to ingested spores. C. botulinum spores are widely present in the environment, including honey. For this reason, it is advised that neither honey, nor any other sweetener, be given to children until after 12 months. Nevertheless, the majority of infants with botulism have no history of ingestion of honey, and the exact source of the offending spores is unclear about 85% of the time. Spores present in the soil are a leading candidate for most cases, and often a history of construction near the home of an affected infant may be obtained.
العلاج
The respiratory failure and paralysis that occur with severe botulism may require a patient to be on a ventilator for weeks, plus intensive medical and nursing care. After several weeks, the paralysis slowly improves. If diagnosed early, foodborne and wound botulism can be treated by inducing passive immunity with a horse-derived antitoxin, which blocks the action of toxin circulating in the blood.[8] This can prevent patients from worsening, but recovery still takes many weeks. Physicians may try to remove contaminated food still in the gut by inducing vomiting or by using enemas. Wounds should be treated, usually surgically, to remove the source of the toxin-producing bacteria. Good supportive care in a hospital is the mainstay of therapy for all forms of botulism.
Besides supportive care, infant botulism can be treated with human botulism immune globulin (BabyBIG), when available. Supply is extremely limited, but is available through the California Department of Health Services. This dramatically decreases the length of illness for most infants. Paradoxically, antibiotics (especially aminoglycosides or clindamycin) may cause dramatic acceleration of paralysis as the affected bacteria release toxin. Visual stimulation should be performed during the time the infant is paralyzed as well, in order to promote the normal development of visual pathways in the brain during this critical developmental period.
Furthermore each case of food-borne botulism is a potential public health emergency in that it is necessary to identify the source of the outbreak and ensure that all persons who have been exposed to the toxin have been identified, and that no contaminated food remains.
There are two primary Botulinum Antitoxins available for treatment of wound and foodborne botulism. Trivalent (A,B,E) Botulinum Antitoxin is derived from equine sources utilizing whole antibodies (Fab & Fc portions). This antitoxin is available from the local health department via the CDC. The second antitoxin is heptavalent (A,B,C,D,E,F,G) Botulinum Antitoxin which is derived from "despeciated" equine IgG antibodies which have had the Fc portion cleaved off leaving the F(ab')2 portions. This is a less immunogenic antitoxin that is effective against all known strains of botulism where not contraindicated. This is available from the US Army. On 1 June, 2006 the US Department of Health and Human Services awarded a $363 million contract with Cangene Corporation for 200,000 doses of Heptavalent Botulinum Antitoxin over five years for delivery into the Strategic National Stockpile beginning in 2007.[9]
المضاعفات
Botulism can result in death due to respiratory failure. However, in the past 50 years, the proportion of patients with botulism who die has fallen from about 50% to 8% due to improved supportive care. A patient with severe botulism may require a breathing machine as well as intensive medical and nursing care for several months. Patients who survive an episode of botulism poisoning may have fatigue and shortness of breath for years and long-term therapy may be needed to aid their recovery.
Infant botulism has no long-term side effects, but can be complicated by nosocomial adverse events. The case fatality rate is less than 1% for hospitalized infants with botulism.
معدل الوفيات
This article may be confusing or unclear to readers. (February 2009) |
Between 1910 and 1919 the death rate from botulism was 70% in the United States, dropping to 9% in the 1980s and 2% in the early 1990s, mainly because of the development of artificial respirators. Up to 60% of botulism cases can be fatal if left untreated.
The World Health Organization (WHO) reports that the current mortality rate is 5% (type B) to 10% (type A). Other sources report that, in the U.S., the overall mortality rate is about 7.5%, but the mortality rate among adults over 60 is 30%. The mortality rate for wound botulism is about 10%. The infant botulism mortality rate is about 1.3%.
Death from botulism is common in waterfowl; an estimated 10 to 100 thousand birds are killed annually. In some large outbreaks, a million or more birds may die. Ducks appear to be affected most often. Botulism also affects commercially raised poultry. In chickens, the mortality rate varies from a few birds to 40% of the flock. Some affected birds may recover without treatment.
Botulism seems to be relatively uncommon in most domestic mammals; however, in some parts of the world, epidemics with up to 65% are seen in cattle. The prognosis is poor in large animals that are recumbent. Most dogs with botulism recover within 2 weeks.
منع العدوى
While commercially canned goods are required to undergo a "botulinum cook" at 121 °C (250 °F) for 3 minutes, and so rarely cause botulism, there have been notable exceptions such as the 1978 Alaskan salmon outbreak and the 2007 Castleberry's Food Co. outbreak. Foodborne botulism has more frequently been from home-canned foods with low acid content, such as carrot juice, asparagus, green beans, beets, and corn. However, outbreaks of botulism have resulted from more unusual sources. In July, 2002, fourteen ألاسكاns ate muktuk (whale meat) from a beached whale, and eight of them developed symptoms of botulism, two of them requiring mechanical ventilation[10]. Other sources of infection include garlic or herbs[11] stored covered in oil without acidification,[12] chile peppers, improperly handled baked potatoes wrapped in aluminium foil [13], and home-canned or fermented fish. Persons who do home canning should follow strict hygienic procedures to reduce contamination of foods. Oils infused with garlic or herbs should be refrigerated. Potatoes which have been baked while wrapped in aluminum foil should be kept hot until served or refrigerated [13]. Because the botulism toxin is destroyed by high temperatures, home-canned foods are best boiled for 20 minutes before eating. Metal cans containing food in which bacteria, possibly botulinum, are growing may bulge outwards due to gas production from bacterial growth; such cans should be discarded. Any container of food which has been heat-treated and then assumed to be airtight which shows signs of not being so, e.g., metal cans with pinprick holes from rust or mechanical damage, should also be discarded.
Wound botulism can be prevented by promptly seeking medical care for infected wounds, and by avoiding punctures by unsterile things such as needles used for street drug injections. It is currently being researched at USAMRIID under BSL-4.
التشخيص
Physicians may consider the diagnosis if the patient's history and physical examination suggest botulism. However, these clues are often not enough to allow a diagnosis of botulism. Other diseases such as Guillain-Barré syndrome, stroke, and myasthenia gravis can appear similar to botulism, and special tests may be needed to exclude these other conditions. These tests may include a brain scan, cerebrospinal fluid examination, nerve conduction test (electromyography, or EMG), and an Edrophonium Chloride (Tensilon) test for myasthenia gravis. A definite diagnosis can be made if botulinum toxin is identified in the feed, stomach or intestinal contents, vomit or feces. The toxin is occasionally found in the blood in peracute cases. Botulinum toxin can be detected by a variety of techniques, including enzyme-linked immunosorbent assays (ELISAs), electrochemiluminescent (ECL) tests and mouse inoculation or feeding trials. The toxins can be typed with neutralization tests in mice. In toxicoinfectious botulism, the organism can be cultured from tissues. On egg yolk medium, toxin-producing colonies usually display surface iridescence that extends beyond the colony.[14]
In cattle, the symptoms may include drooling, restlessness, uncoordination, urine retention, dysphagia, and sternal recumbency. Laterally recumbent animals are usually very close to death. In sheep, the symptoms may include drooling, a serous nasal discharge, stiffness, and inco-ordination. Abdominal respiration may be observed and the tail may switch on the side. As the disease progresses, the limbs may become paralysed and death may occur.
The clinical signs in horses are similar to cattle. The muscle paralysis is progressive; it usually begins at the hindquarters and gradually moves to the front limbs, neck, and head. Death generally occurs 24 to 72 hours after initial symptoms and results from respiratory paralysis. Some foals are found dead without other clinical signs.
Pigs are relatively resistant to botulism. Reported symptoms include anorexia, refusal to drink, vomiting, pupillary dilation, and muscle paralysis.[15]
In poultry and wild birds, flaccid paralysis is usually seen in the legs, wings, neck and eyelids. Broiler chickens with the toxicoinfectious form may also have diarrhoea with excess urates.
انظر أيضا
- List of foodborne illness outbreaks
- Botox
- Centers for Disease Control and Prevention (CDC)
- Castleberry's Food Company
المراجع
- ^ أ ب ت ث ج ح خطأ استشهاد: وسم
<ref>غير صحيح؛ لا نص تم توفيره للمراجع المسماةWHO2018 - ^ أ ب ت "Consumers - Foodborne Illnesses: What You Need to Know". FDA (in الإنجليزية). Retrieved 11 May 2018.
- ^ Caterino, Jeffrey M.; Kahan, Scott (2003). In a Page: Emergency medicine. Lippincott Williams & Wilkins. p. 122. ISBN 9781405103572.
{{cite book}}: Unknown parameter|name-list-format=ignored (|name-list-style=suggested) (help) - ^ Passaro DJ, Werner SB, McGee J, Mac Kenzie WR, Vugia DJ. Wound botulism associated with black tar heroin among injecting drug users. JAMA 1998;279:859-63. PMID 9516001.
- ^ Clostridium botulinum Outbreak | CDC Botulism
- ^ FDA Warns of Potential Botulism Risk from Canned French Cut Green Beans Product Marketed Under a Variety of Brand Names
- ^ Oxford Textbook of Medicine, 4th Ed., Section 7.55
- ^ Shapiro, Roger L. MD; Charles Hatheway, PhD; and David L. Swerdlow, MD Botulism in the United States: A Clinical and Epidemiologic Review Annals of Internal Medicine. 1 August 1998 Volume 129 Issue 3 Pages 221-228
- ^ http://mmrs.fema.gov/news/publichealth/2006/aug/nph2006-08-03a.aspx قالب:Citation broken
- ^ Outbreak of Botulism Type E Associated with Eating a Beached Whale --- Western Alaska, July 2002, CDC Morbidity and Mortality Weekly Report, January 17, 2003
- ^ Oil Infusions and the Risk of Botulism, Colorado State University Cooperative Extension, Safefood new - Summer 1998 - Vol 2 / No. 4
- ^ Update: International Outbreak of Restaurant-Associated Botulism -- Vancouver, British Columbia, Canada, CDC Morbidity and Mortality Weekly Report, October 18, 1985
- ^ أ ب "Botulism Linked to Baked Potatoes". Retrieved 2007-03-21.
- ^ Weber,J.T. "Botulism" In Infectious Diseases, 5th ed. Edited by P.D. Hpeprich, J.B. Lippincott Company, 1994, pp. 1185-1194.
- ^ "Botulism." In the Merck Veterinary Manual, 8th ed. Edited by S.E. Aiello and A. Mays. Whitehouse Station, NJ: Merck and CO., 1988, pp.442-444.
إطلاعات أخرى
- Clostridium Botulinum In The Food Chain, By Dr. Rhodri Evans, Department of Industrial Microbiology, University College, Dublin, Belfield, Dublin 4. Published in Hygiene Review 1997, under the auspices of The Society of Food Hygiene Technology.
الروابط الخارجية
- Agent Fact Sheet: Botulism, Center for Biosecurity
- Botulism (Technical information from the CDC)
- Infant Botulism Treatment and Prevention Program
- Clostridium Botulinum (FDA/CFSAN)
- Botulism (WHO)
- Avian Botulism