مضاد الذهان
| أسيل ساهم بشكل رئيسي في تحرير هذا المقال
|
يستعمل مصطلح مضادات الذهان[1] للدلالة على مجموعة أدوية تستعمل لمعالجة الذهان إنگليزية: psychosis أو ما يمكن تسميته بالاضطرابات النفسية، التي تشمل الفصام (انفصام الشخصية) إنگليزية: schizophrenia، اضطرابات التوهم إنگليزية: delusional disorder، الجنون (الهوس) إنگليزية: mania، قد تستخدم أيضا لعلاج حالات ذهانية أخرى تترافق مع أعراض أخرى.
لمضادات الذهان أيضا دور كمصححات مزاجية إنگليزية: mood stabilizer مما يدفع لاستخدامها أيضا في علاج اضطرابات المزاج إنگليزية: mood disorder بالأخص الاضطرابات ثنائية القطبية إنگليزية: bipolar disorder (حتى لو تترافق هذه الأمراض مع أي من عوارض الذهان). بعض هذه الدوية أيضا مثل هالوبيريدول، وبيموزيد يستخدم في علاج متلازمة توريت إنگليزية: Tourette's Syndrome.
يشار لمضادات الذهان أيضا باسم منعشات عصبية إنگليزية: neuroleptics أو الأدوية المنعشة عصبيا (اقرأ المنعشات).
تقسم مضادات الذهان عادة إلى : مضادات ذهان نموذجية (نمطية) ولانموذجية. المضادات الذهانية النموذجية يشار لها عادة بالمهدئات العامة أو المهدئات الكبرى (المطمئنات الكبرى) إنگليزية: major tranquilizers بسبب تأثيرها المهديء والمطمئن عندما تأخذ بجرعات كبيرة. لكن هذه التسمية تم إهمالها مؤخرا كثيرا لأن العديد من مضادات الذهان ليس لها تأثيرا مهدئا كبيرا كما إن هذا المصطلح كان يوحي بنوع مع العلاقة مع بنزوديازبين ومشتقاته (أو ما كان يسمى بالمهدئات الصغرى)، في حين أن هذه العلاقة غير موجودة.
التاريخ
The original antipsychotic drugs were happened upon largely by chance and then tested for their effectiveness. The first, chlorpromazine, was developed as a surgical anesthetic. It was first used on psychiatric patients because of its powerful calming effect; at the time it was regarded as a "chemical lobotomy". Lobotomy at the time was used to treat many behavioral disorders, including psychosis, although its effect was to markedly reduce behavior and mental functioning of all types. However, chlorpromazine proved to reduce the effects of psychosis in a more effective and specific manner than the extreme lobotomy-like sedation it was known for. The underlying neurochemistry involved has since been studied in detail, and subsequent antipsychotic drugs have been discovered by an approach that incorporates this sort of information.
Antipsychotics have long been known as neuroleptic drugs.[2] The word neuroleptic was derived from the باليونانية: "νεῦρον" (neuron, originally meaning "sinew" but today referring to the nerves) and "λαμβάνω" (lambanō, meaning "take hold of"). Thus, the word means taking hold of one's nerves. This may refer to common side effects such as reduced activity, lethargy, and impaired motor control. Although these effects are unpleasant and in some cases harmful, they were at one time considered a reliable sign that the drug was working.[بحاجة لمصدر] The term "neuroleptic" is being abandoned in favor of "antipsychotic," which refers to the drug's desired effects. Typical antipsychotics have also been referred to as the major tranquilizers,[3] because of their tendency to tranquilize and sedate. As with the term "neuroleptics," the term "major tranquilizers" is falling out of common and scientific use. The term "tranquilizers" now generally refers to drugs that are primarily intended to sedate—mostly the barbiturates and benzodiazepines, which were once referred to as the "minor tranquilizers."
Antipsychotics are broadly divided into two groups, the typical or first-generation antipsychotics and the atypical or second-generation antipsychotics. The typical antipsychotics are classified according to their chemical structure while the atypical antipsychotics are classified according to their pharmacological properties. These include serotonin-dopamine antagonists (see dopamine antagonist and serotonin antagonist), multi-acting receptor-targeted antipsychotics (MARTA, those targeting several systems), and dopamine partial agonists, which are often categorized as atypicals.[4]
According to the UK Guardian newspaper: "At the heart of years of dissent against psychiatry through the ages has been its use of drugs, particularly antipsychotics, to treat distress. Do such drugs actually target any "psychiatric condition"? Or are they chemical control - a socially-useful reduction of the paranoid, deluded, distressed, bizarre and odd into semi-vegetative zombies?"[5]
الاستخدام
Common conditions with which antipsychotics might be used include schizophrenia, bipolar disorder and delusional disorder. Antipsychotics might also be used to counter psychosis associated with a wide range of other diagnoses, such as psychotic depression.
In addition, "antipsychotics" are increasingly used to treat non-psychotic disorders. For example, they are sometimes used off-label to manage aspects of Tourette syndrome or autism spectrum disorders. They have multiple off-label uses as an augmentation agent (i.e. in addition to another medication), for example in "treatment-resistant" depression[6] or OCD.[7] Despite the name, the off-label use of "antipsychotics" is said to involve deploying them as antidepressants, anti-anxiety drugs, mood stabilizers, cognitive enhancers, anti-aggressive, anti-impulsive, anti-suicidal and hypnotic (sleep) medications.[8]
Antipsychotics have also been increasingly used off-label in cases of dementia in older people, and for various disorders and difficulties in children and teenagers. A survey of children with pervasive developmental disorder found that 16.5% were taking an antipsychotic drug, most commonly to alleviate mood and behavioral disturbances characterized by irritability, aggression, and agitation. Recently, risperidone was approved by the US FDA for the treatment of irritability in children and adolescents with autism.[9]
Antipsychotics are sometimes used as part of compulsory treatment via inpatient (hospital) commitment or outpatient commitment. This may involve various methods to persuade a person to take the medication, or actual physical force. Administration may rely on an injectable form of the drug rather than tablets. The injection may be of a long-lasting type known as a depot injection, usually applied at the top of the buttocks.
Antipsychotics are among the biggest selling and most profitable of all drugs, generating $22 billion in global sales in 2008.[10] By 2003 in the US, an estimated 3.21 million patients received antipsychotics, worth an estimated $2.82 billion. Over 2/3 of prescriptions were for the newer more expensive atypicals, each costing on average $164 compared to $40 for the older types.[11] By 2008, sales in the US reached $14.6 billion, the biggest selling drugs in the US by therapeutic class.[12] The number of prescriptions for children and adolescents doubled to 4.4 million between 2003 and 2006, in part because of increases in diagnoses of bipolar disorder.[13]
الآثار الجانبية
Antipsychotics are associated with a range of side effects. It is well-recognized that many people stop taking them (around two-thirds even in controlled drug trials) due in part to adverse effects.[14] Extrapyramidal reactions include acute dystonias, akathisia, parkinsonism (rigidity and tremor), tardive dyskinesia, tachycardia, hypotension, impotence, lethargy, seizures, intense dreams or nightmares, and hyperprolactinaemia.[15] Some of the side-effects will appear after the drug has been used only for a long time.
The most serious adverse effect associated with long-term antipsychotic use is lowered life expectancy. This has proved most controversial in regard to the use of antipsychotics in dementia in older people, worsened by alleged use to control and sedate rather than necessarily to treat. A 2009 systematic review of studies of schizophrenia also found decreased life expectancy associated with use of antipsychotics and argued that more studies were urgently needed,[16] a call that had already been made when similar results were found in 2006.[17]
In "healthy" individuals without psychosis, doses of antipsychotics can produce the so-called "negative symptoms" (e.g. emotional and motivational difficulties) associated with schizophrenia.[18]
From a subjective perspective, antipsychotics heavily influence one's perceptions of pleasurable sensations, causing a severe reduction in feelings of desire, motivation, pensive thought, and awe. This does not coincide with the apathy and lack of motivation experienced by the negative symptoms of schizophrenia. Detrimental effects on short term memory, which affect the way one figures and calculates (although this also may be purely subjective), may also be observed on high enough dosages. These are all the reasons why they are thought to affect "creativity". Also, for some individuals with schizophrenia, too much stress may cause "relapse".
Following are details concerning some of the side effects of antipsychotics:
- Antipsychotics, particularly atypicals, appear to cause diabetes mellitus and fatal diabetic ketoacidosis, especially (in US studies) in African Americans.[19][20]
- Antipsychotics may cause pancreatitis.[21]
- The atypical antipsychotics (especially olanzapine) seem to cause weight gain more commonly than the typical antipsychotics. The well-documented metabolic side effects associated with weight gain include diabetes, which can be life-threatening.[22]
- Antipsychotics increase the likelihood of a fatal heart attack, with the risk of death increasing with dose and the length of time on the drug.[23]
- Clozapine also has a risk of inducing agranulocytosis, a potentially dangerous reduction in the number of white blood cells in the body. Because of this risk, patients prescribed clozapine may need to have regular blood checks to catch the condition early if it does occur, so the patient is in no danger.[24]
- One of the more serious of these side effects is tardive dyskinesia, in which the sufferer may show repetitive, involuntary, purposeless movements often of the lips, face, legs, or torso. It is believed that there is a greater risk of developing tardive dyskinesia with the older, typical antipsychotic drugs, although the newer antipsychotics are now also known to cause this disorder.
- A potentially serious side effect of many antipsychotics is that they tend to lower an individual's seizure threshold. Chlorpromazine and clozapine, in particular, have a relatively high seizurogenic potential. Fluphenazine, haloperidol, pimozide and risperidone exhibit a relatively low risk. Caution should be exercised in individuals that have a history of seizurogenic conditions such as epilepsy, or brain damage.
- Neuroleptic malignant syndrome, in which the drugs appear to cause the temperature regulation centers to fail, resulting in a medical emergency, as the patient's temperature suddenly increases to dangerous levels.
- Dysphoria.
- Sexual dysfunction.
- Dystonia - a neurological movement disorder in which sustained muscle contractions cause twisting and repetitive movements or abnormal postures.
- Hyperprolactinaemia - The breasts may enlarge and discharge milk, in both men and women due to abnormally-high levels of prolactin in the blood. Prolactin secretion in the pituitary is normally suppressed by dopamine. Drugs that block the effects of dopamine at the pituitary or deplete dopamine stores in the brain may cause the pituitary to secrete prolactin.
- There is evidence that exposure may cause demyelinating disease in laboratory animals.[25]
- Following controversy over possible increased mortality (death) related to antipsychotics in indivdiuals with dementia, warnings have been added to packaging.[26]
Some people suffer few apparent side effects from taking antipsychotic medication, whereas others may have serious adverse effects. Some side effects, such as subtle cognitive problems, may go unnoticed.
There is a possibility that the risk of tardive dyskinesia can be reduced by combining the anti-psychotics with diphenhydramine or benzatropine, although this remains to be established. Central nervous system damage is also associated with irreversible tardive akathisia and/or tardive dysphrenia.
انسحاب الدواء
Withdrawal symptoms from antipsychotics may emerge during dosage reduction and discontinuation. Withdrawal symptoms can include nausea, emesis, anorexia, diarrhea, rhinorrhea, diaphoresis, myalgia, paresthesia, anxiety, agitation, restlessness, and insomnia. The psychological withdrawal symptoms can include psychosis, and can be mistaken for a relapse of the underlying disorder. Conversely, the withdrawal syndrome may also be a trigger for relapse. Better management of the withdrawal syndrome may improve the ability of individuals to discontinue antipsychotics.[27][28]
Tardive dyskinesia can emerge as a physical withdrawal symptom, and may either gradually abate during the withdrawal phase, or become persistent.[29] Withdrawal-related psychosis from antipsychotics is called "supersensitivity psychosis", and is attributed to increased number and sensitivity of brain dopamine receptors, due to blockade of dopaminergic receptors by the antipsychotics,[30] which often leads to exacerbated symptoms in the absence of neuroleptic medication[31]. Efficacy of antipsychotics may likewise be reduced over time, due to this development of drug tolerance.[28]
Withdrawal effects may also occur when switching a person from one antipsychotic to another, (presumably due to variations of potency and receptor activity). Such withdrawal effects can include cholinergic rebound, an activation syndrome, and motor syndromes including dyskinesias. These adverse effects are more likely during rapid changes between antipsychotic agents, so making a gradual change between antipsychotics minimises these withdrawal effects.[32] The British National Formulary recommends a gradual withdrawal when discontinuing antipsychotic treatment to avoid acute withdrawal syndrome or rapid relapse.[33]
التأثير
There have been a large number of studies of the efficacy of typical antipsychotics, and an increasing number on the more recent atypical antipsychotics.
The American Psychiatric Association and the UK National Institute for Health and Clinical Excellence recommend antipsychotics for managing acute psychotic episodes in schizophrenia or bipolar disorder, and as a longer-term maintenance treatment for reducing the likelihood of further episodes.[34][35] They state that response to any given antipsychotic can be variable so that trials may be necessary, and that lower doses are to be preferred where possible. A number of studies have looked at levels of "compliance" or "adherence" with antipsychotic regimes and found that discontinuation (stopping taking them) by patients is associated with higher rates of relapse, including hospitalization.
Nevertheless, a 2009 systematic review and meta-analysis of trials in people diagnosed with schizophrenia found that less than half (41%) showed any therapeutic response to an antipsychotic, compared to 24% on placebo, and that there was a decline in treatment response over time, and possibly a bias in which trial results were published.[36] In addition, a 2010 Cochrane Collaboration review of trials of Risperidone, one of the biggest selling antipsychotics and the first of the new generation to become available in generic form, found only marginal benefit compared with placebo and that, despite its widespread use, evidence remains limited, poorly reported and probably biased in favor of risperidone due to pharmaceutical company funding of trials.[37] Another Cochrane review in 2009, of bipolar disorder, found the efficacy and risk/benefit ratio better for the traditional mood stabilizer lithium than for the antipsychotic Olanzapine as a first line maintenance treatment.[38]
Antipsychotic polypharmacy (prescribing two or more antipsychotics at the same time for an individual) is said to be a common practice but not necessarily evidence-based or recommended, and there have been initiatives to curtail it.[39] Similarly, the use of excessively high doses (often the result of polypharmacy) continues despite clinical guidelines and evidence indicating that it is usually no more effective but is usually more harmful.[40]
A review by the US Agency for Healthcare Research and Quality found that much of the evidence for the off-label use of antipsychotics (for example, for depression, dementia, OCD, PTSD, Personality Disorders, Tourette's) was of insufficient scientific quality to support such use, especially as there was strong evidence of increased risks of stroke, tremors, significant weight gain, sedation, and gastrointestinal problems.[41] A UK review of unlicensed usage in children and adolescents reported a similar mixture of findings and concerns.[42]
Aggressive challenging behavior in adults with intellectual disability is often treated with antipsychotic drugs despite lack of an evidence base. A recent randomized controlled trial, however, found no benefit over placebo and recommended that the use of antipsychotics in this way should no longer be regarded as an acceptable routine treatment.[43]
A 2006 Cochrane Collaboration review of controlled trials of antipsychotics in old age dementia reported that one or two of the drugs showed a modest benefit compared to placebo in managing aggression or psychosis, but that this was combined with a significant increase in serious adverse events. They concluded that this confirms that antipsychotics should not be used routinely to treat dementia patients with aggression or psychosis, but may be an option in the minority of cases where there is severe distress or risk of physical harm to others.[44]
Some doubts have been raised about the long-term effectiveness of antipsychotics for schizophrenia, in part because two large international World Health Organization studies found individuals diagnosed with schizophrenia tend to have better long-term outcomes in developing countries (where there is lower availability and use of antipsychotics) than in developed countries.[45][46] The reasons for the differences are not clear, however, and various explanations have been suggested.
Some argue that the evidence for antipsychotics from discontinuation-relapse studies may be flawed, because they do not take into account that antipsychotics may sensitize the brain and provoke psychosis if discontinued, which may then be wrongly interpreted as a relapse of the original condition.[47] Evidence from comparison studies indicates that at least some individuals with schizophrenia recover from psychosis without taking antipsychotics, and may do better in the long-term than those that do take antipsychotics.[48] Some argue that, overall, the evidence suggests that antipsychotics only help if they are used selectively and are gradually withdrawn as soon as possible[49] and have referred to the "Myth of the antipsychotic".[50]
A review of the methods used in trials of antipsychotics, despite stating that the overall quality is "rather good," reported issues with the selection of participants (including that in schizophrenia trials up to 90% of people who are generally suitable do not meet the elaborate inclusion and exclusion criteria, and that negative symptoms have not been properly assessed despite companies marketing the newer antipsychotics for these); issues with the design of trials (including pharmaceutical company funding of most of them, and inadequate experimental "blinding" so that trial participants could sometimes tell whether they were on placebo or not); and issues with the assessment of outcomes (including the use of a minimal reduction in scores to show "response," lack of assessment of quality of life or recovery, a high rate of discontinuation, selective highlighting of favorable results in the abstracts of publications, and poor reporting of side-effects).[51]
Typicals versus atypicals
While the atypical (second-generation) antipsychotics were marketed as offering greater efficacy in reducing psychotic symptoms while reducing side effects (and Extrapyramidal symptoms in particular) than typical medications, the results showing these effects often lacked robustness, and the assumption was increasingly challenged even as atypical prescriptions were soaring.[52] One review concluded there were no differences[4] while another[53] found that atypicals were "only moderately more efficacious".[4] These conclusions were, however, questioned by another review, which found that clozapine, amisulpride, and olanzapine and risperidone were more effective[4][54] Clozapine has appeared to be more effective than other atypical antipsychotics,[4][55] although it has previously been banned due to its potentially lethal side effects. While controlled clinical trials of atypicals reported that extrapyramidal symptoms occurred in 5–15% of patients, a study of bipolar disorder in a real world clinical setting found a rate of 63%, questioning the generalizability of the trials.[56]
In 2005 the US government body NIMH published the results of a major independent (not funded by the pharmaceutical companies) multi-site, double-blind study (the CATIE project).[57] This study compared several atypical antipsychotics to an older typical antipsychotic, perphenazine, among 1493 persons with schizophrenia. The study found that only olanzapine outperformed perphenazine in discontinuation rate (the rate at which people stopped taking it due to its effects). The authors noted an apparent superior efficacy of olanzapine to the other drugs in terms of reduction in psychopathology and rate of hospitalizations, but olanzapine was associated with relatively severe metabolic effects such as a major weight gain problem (averaging 44 pounds over 18 months) and increases in glucose, cholesterol, and triglycerides. No other atypical studied (risperidone, quetiapine, and ziprasidone) did better than the typical perphenazine on the measures used, nor did they produce fewer adverse effects than the typical antipsychotic perphenazine (a result supported by a meta-analysis by Dr. Leucht published in Lancet), although more patients discontinued perphenazine owing to extrapyramidal effects compared to the atypical agents (8% vs. 2% to 4%, P=0.002).
A phase 2 part of this CATIE study roughly replicated these findings.[58] This phase consisted of a second randomization of the patients that discontinued taking medication in the first phase. Olanzapine was again the only medication to stand out in the outcome measures, although the results did not always reach statistical significance (which means they were not reliable findings) due in part to the decrease of power. The atypicals again did not produce fewer extrapyramidal effects than perphenazine. A subsequent phase was conducted[59] that allowed clinicians to offer clozapine which was more effective at reducing medication drop-outs than other neuroleptic agents. However, the potential for clozapine to cause toxic side effects, including agranulocytosis, limits its usefulness.
It had been hoped that patient adherence to antipsychotics would be higher with the atypicals, but a 2008 review found that the data have failed to substantiate the notion that novel antipsychotic drug use leads to improved medication compliance and favorable clinical outcomes.[60]
Overall evaluations of the CATIE and other studies have led many researchers to question the first-line prescribing of atypicals over typicals, or even to question the distinction between the two classes.[61][62] The UK government organization NICE recently revised its recommendation favoring atypicals, to advise that the choice should be an individual one based on the particular profiles of the individual drug and on the patient's preferences.
The re-evaluation of the evidence has not necessarily slowed the bias towards prescribing the atypicals, however.[63]
مضادات الذهان الشائعة
Commonly used antipsychotic medications are listed below by drug group. Trade names appear in parentheses.
الجيل الأول من مضادات الذهان
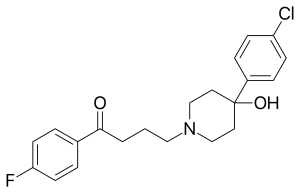
Butyrophenones
- Haloperidol (Haldol, Serenace)
- Droperidol (Droleptan)
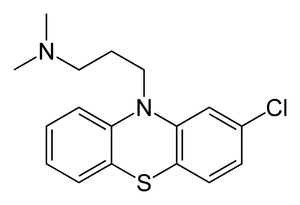
فنوثيازينات
- Chlorpromazine (Thorazine, Largactil)
- Fluphenazine (Prolixin) - Available in decanoate (long-acting) form
- Perphenazine (Trilafon)
- Prochlorperazine (Compazine)
- Thioridazine (Mellaril, Melleril)
- Trifluoperazine (Stelazine)
- Mesoridazine
- Periciazine
- Promazine
- Triflupromazine (Vesprin)
- Levomepromazine (Nozinan)
- Promethazine (Phenergan)
- Pimozide (Orap)
الثيوكسانثنات
- Chlorprothixene (Cloxan, Taractan, Truxal)
- Clopenthixol (Sordinol)
- Flupenthixol (Depixol, Fluanxol)
- Thiothixene (Navane)
- Zuclopenthixol (Cisordinol, Clopixol, Acuphase)
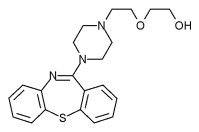
الجيل اثاني من مضادات الذهان
- Clozapine (Clozaril) - Requires weekly to biweekly complete blood count due to risk of agranulocytosis.
- Olanzapine (Zyprexa) - Used to treat psychotic disorders including schizophrenia, acute manic episodes, and maintenance of bipolar disorder. Dosing 2.5 to 20 mg per day.
- Risperidone (Risperdal) - Dosing 0.25 to 6 mg per day and is titrated upward; divided dosing is recommended until initial titration is completed, at which time the drug can be administered once daily. Used off-label to treat Tourette syndrome and anxiety disorder.
- Quetiapine (Seroquel) - Used primarily to treat bipolar disorder and schizophrenia, and "off-label" to treat chronic insomnia and restless legs syndrome; it is a powerful sedative. Dosing starts at 25 mg and continues up to 800 mg maximum per day, depending on the severity of the symptom(s) being treated.
- Ziprasidone (Geodon) - Approved in 2006[بحاجة لمصدر] to treat bipolar disorder. Dosing 20 mg twice daily initially up to 80 mg twice daily. Side-effects include a prolonged QT interval in the heart, which can be dangerous for patients with heart disease or those taking other drugs that prolong the QT interval.
- Amisulpride (Solian) - Selective dopamine antagonist. Higher doses (greater than 400 mg) act upon post-synaptic dopamine receptors resulting in a reduction in the positive symptoms of schizophrenia, such as psychosis. Lower doses, however, act upon dopamine autoreceptors, resulting in increased dopamine transmission, improving the negative symptoms of schizophrenia. Lower doses of amisulpride have also been shown to have antidepressant and anxiolytic effects in non-schizophrenic patients, leading to its use in dysthymia and social phobias. Amisulpride has not been approved for use by the Food and Drug Administration in the United States.
- Asenapine (Saphris) is a 5-HT2A- and D2-receptor antagonist under development for the treatment of schizophrenia and acute mania associated with bipolar disorder.
- Paliperidone (Invega) - Derivative of risperidone that was approved in 2006.
- Iloperidone (Fanapt) - Approved by the FDA on May 6, 2009.
- Zotepine (Nipolept, Losizopilon, Lodopin, Setous)- An atypical antipsychotic indicated for acute and chronic schizophrenia. It was approved in Japan circa 1982 and Germany in 1990, respectively.
- Sertindole (Serdolect, and Serlect in Mexico). Sertindole was developed by the Danish pharmaceutical company H. Lundbeck. Like the other atypical antipsychotics, it is believed to have antagonist activity at dopamine and serotonin receptors in the brain.
الجيل الثالث من مضادات الذهان
- Aripiprazole (Abilify) - Dosing 1 mg up to maximum of 30 mg has been used. Mechanism of action is thought to reduce susceptibility to metabolic symptoms seen in some other atypical antipsychotics.[64] The extent to which these effects differ from other atypical antipsychotics is debated.[65]
- Partial agonists of dopamine.
- Under clinical development - Bifeprunox.
إمكانيات أخرى
- Cannabidiol is one of the main psychoactive components of cannabis. A recent study has shown that cannabidiol may be as effective as atypical antipsychotics in treating schizophrenia.[66] Further research has supported these results, and found fewer side effects with cannabidiol than with amisulpride.[67][67]
- Tetrabenazine is similar in function to antipsychotic drugs, though is not, in general, considered an antipsychotic itself. Its main usefulness is the treatment of hyperkinetic movement disorders such as Huntington's disease and Tourette syndrome, rather than for conditions such as schizophrenia. Also, rather than having the potential to cause tardive dyskinesia, which most antipsychotics have, tetrabenazine can be an effective treatment for the condition.
- Metabotropic glutamate receptor 2 agonism has been seen as a promising strategy in the development of novel antipsychotics.[68][69][70] When tested in patients, the research substance LY2140023 yielded promising results and had few side effects. The active metabolite of this prodrug targets the brain glutamate receptors mGluR2/3 rather than dopamine receptors.[71]
عمل الدواء
All antipsychotic drugs tend to block D2 receptors in the dopamine pathways of the brain. This means that dopamine released in these pathways has less effect. Excess release of dopamine in the mesolimbic pathway has been linked to psychotic experiences. It is the blockade of dopamine receptors in this pathway that is thought to control psychotic experiences.
Typical antipsychotics are not particularly selective and also block dopamine receptors in the mesocortical pathway, tuberoinfundibular pathway, and the nigrostriatal pathway. Blocking D2 receptors in these other pathways is thought to produce some of the unwanted side effects that the typical antipsychotics can produce (see below). They were commonly classified on a spectrum of low potency to high potency, where potency referred to the ability of the drug to bind to dopamine receptors, and not to the effectiveness of the drug. High-potency antipsychotics such as haloperidol, in general, have doses of a few milligrams and cause less sleepiness and calming effects than low-potency antipsychotics such as chlorpromazine and thioridazine, which have dosages of several hundred milligrams. The latter have a greater degree of anticholinergic and antihistaminergic activity, which can counteract dopamine-related side effects.
Atypical antipsychotic drugs have a similar blocking effect on D2 receptors. Some also block or partially block serotonin receptors (particularly 5HT2A, C and 5HT1A receptors):ranging from risperidone, which acts overwhelmingly on serotonin receptors, to amisulpride, which has no serotonergic activity. The additional effects on serotonin receptors may be why some of them can benefit the "negative symptoms" of schizophrenia.[72]
التأثيريات التركيبية
Many studies now indicate that chronic treatment with antipsychotics affects the brain at a structural level, for example increasing the volume of the basal ganglia (especially the caudate nucleus), and reducing cortical grey matter volume in different brain areas. The effects may differ for typical versus atypical antipsychotics and may interact with different stages of disorders.[73] Death of neurons in the cerebral cortex, especially in women, has been linked to the use of both typical and atypical antipsychotics for individuals with Alzheimers.[74]
Recent studies on macaque monkeys have found that administration of haloperidol or olanzapine for about two years led to a significant overall shrinkage in brain tissue,[75] in both gray and white matter across several brain areas, with lower glial cell counts,[76] due to a decrease in astrocytes and oligodendrocytes,[77] and increased neuronal density. It has been said that these studies require serious attention and that such effects were not clearly tested for by pharmaceutical companies prior to obtaining approval for placing the drugs on the market.[78]
نقد
Use of this class of drugs has a history of criticism in residential care. As the drugs used can make patients calmer and more compliant, critics claim that the drugs can be overused. Outside doctors can feel under pressure from care home staff.[79] In an official review commissioned by UK government ministers it was reported that the needless use of anti-psychotic medication in dementia care was widespread and was linked to 1800 deaths per year.[80][81] In the US, the government has initiated legal action against the pharmaceutical company Johnson & Johnson for allegedly paying kickbacks to Omnicare to promote its antipsychotic Risperidone (Risperdal) in nursing homes.[82]
There is some controversy over maintenance therapy for schizophrenia.[28][83] A review of studies about maintenance therapy concluded that long-term antipsychotic treatment was superior to placebo in reducing relapse in individuals with schizophrenia, although some of the studies were small.[84] A review of major longitudinal studies in North America found that a moderate number of patients with schizophrenia were seen to recover over time from their symptoms, raising the possibility that some patients may not require maintenance medication.[83] It has also been argued that much of the research into long-term antipsychotic maintenance may be flawed due to failure to take into account the role of antipsychotic withdrawal effects on relapse rates.[28]
There has also been controversy about the role of pharmaceutical companies in marketing and promoting antipsychotics, including allegations of downplaying or covering up adverse effects, expanding the number of conditions or illegally promoting off-label usage; influencing drug trials (or their publication) to try to show that the expensive and profitable newer atypicals were superior to the older cheaper typicals that were out of patent. For example in the US, Eli Lilly recently pleaded guilty to violating US laws for over a decade in regard to Zyprexa (olanzapine), and was ordered to pay $1.42 billion to settle criminal and civil allegations, including the biggest criminal fine for an individual corporation ever imposed in US history; while Astrazeneca is facing about 9,000 personal-injury lawsuits from more than 15,000 former users of Seroquel (quetiapine), amidst federal investigations of its marketing practices.[85] By expanding the conditions for which they were indicated, Astrazeneca's Seroquel and Eli Lilly's Zyprexa had become the biggest selling antipsychotics in 2008 with global sales of $5.5 billion and $5.4 billion respectively.[10]
Some critics have also analyzed the use of alleged front organizations and conflicted patient "advocacy" groups funded by pharmaceutical companies that seek to set the mental health agenda, including the use of the law to force people to take antipsychotics against their will, often justified by claims about risk of violence.[86]
المصادر
- ^ الويكيبيديا الموسوعة الحرة
- ^ "neuroleptic" في قاموس دورلاند الطبي
- ^ "tranquilizer" في قاموس دورلاند الطبي
- ^ أ ب ت ث ج Horacek J, Bubenikova-Valesova V, Kopecek M; et al. (2006). "Mechanism of action of atypical antipsychotic drugs and the neurobiology of schizophrenia". CNS Drugs. 20 (5): 389–409. doi:10.2165/00023210-200620050-00004. PMID 16696579.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) - ^ Myth of the antipsychotic
- ^ Docs.Google.com
- ^ A Review of Antipsychotics in the Treatment of Obsessive Compulsive Disorder (2007)
- ^ Groleger U (2007). "Off-label use of antipsychotics: rethinking 'off-label'". Psychiatria Danubina. 19 (4): 350–3. PMID 18000487.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Antipsychotics in the treatment of autism (2008)
- ^ أ ب Pipeline antipsychotic drugs to drive next market evolution (2009)
- ^ Antipsychotic Use and Expenditure in the United States (2006)
- ^ 2008 U.S. Sales and Prescription Information: Top Therapeutic Classes by U.S. Sales (PDF)
- ^ Newer antipsychotic drugs draw fresh scrutiny (2009)
- ^ Bellack AS (2006). "Scientific and consumer models of recovery in schizophrenia: concordance, contrasts, and implications". Schizophrenia Bulletin. 32 (3): 432–42. doi:10.1093/schbul/sbj044. PMC 2632241. PMID 16461575.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Mangrella M, Motola G, Russo F; et al. (1998). "[Intensive hospital monitoring of adverse reactions to benzodiazepines and neuroleptic agents]". Minerva Medica (in Italian). 89 (7–8): 293–300. PMID 9824992.
{{cite journal}}: Explicit use of et al. in:|author=(help)CS1 maint: multiple names: authors list (link) CS1 maint: unrecognized language (link) - ^ Influence of antipsychotics on mortality in schizophrenia: Systematic review (2009)
- ^ Schizophrenia, neuroleptic medication and mortality (2006)
- ^ Negative Signs and Symptoms Secondary to Antipsychotics: A Double-Blind, Randomized Trial of a Single Dose of Placebo, Haloperidol, and Risperidone in Healthy Volunteers (2006)
- ^ Torrey EF, Swalwell CI (2003). "Fatal olanzapine-induced ketoacidosis". The American Journal of Psychiatry. 160 (12): 2241. doi:10.1176/appi.ajp.160.12.2241. PMID 14638601.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Koller EA, Doraiswamy PM (2002). "Olanzapine-associated diabetes mellitus". Pharmacotherapy. 22 (7): 841–52. doi:10.1592/phco.22.11.841.33629. PMID 12126218.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Koller EA, Cross JT, Doraiswamy PM, Malozowski SN (2003). "Pancreatitis associated with atypical antipsychotics: from the Food and Drug Administration's MedWatch surveillance system and published reports". Pharmacotherapy. 23 (9): 1123–30. doi:10.1592/phco.23.10.1123.32759. PMID 14524644.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Hasnain M, Vieweg WVR, Fredrickson SK (2010). "Metformin for Atypical Antipsychotic-Induced Weight Gain and Glucose Metabolism Dysregulation: Review of the Literature and Clinical Suggestions". CNS Drugs. 24 (3): 193–206. doi:10.2165/11530130-000000000-00000.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Newer antipsychotic drugs draw fresh scrutiny (2008)
- ^ Baldessarini, Ross J. (2006). "Pharmacotherapy of Psychosis and Mania". In Laurence Brunton, John Lazo, Keith Parker (eds.) (ed.). Goodman & Gilman's The Pharmacological Basis of Therapeutics (11th ed.). New York: McGraw-Hill. ISBN 978-0071422802. OCLC 150149056.
{{cite book}}:|editor=has generic name (help); Unknown parameter|coauthors=ignored (|author=suggested) (help)CS1 maint: multiple names: editors list (link)[صفحة مطلوبة] - ^ Konopaske GT, Dorph-Petersen KA, Sweet RA; et al. (2008). "Effect of chronic antipsychotic exposure on astrocyte and oligodendrocyte numbers in macaque monkeys". Biological Psychiatry. 63 (8): 759–65. doi:10.1016/j.biopsych.2007.08.018. PMC 2386415. PMID 17945195.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Glever, J (2008). "Boxed Mortality Warning Added to Older Antipsychotics Given to Elderly Demented". Medpage Today. Retrieved 2009-04-24.
- ^ Dilsaver, SC.; Alessi, NE. (1988). "Antipsychotic withdrawal symptoms: phenomenology and pathophysiology". Acta Psychiatr Scand. 77 (3): 241–6. PMID 2899377.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ أ ب ت ث Moncrieff, J. (2006). "Why is it so difficult to stop psychiatric drug treatment? It may be nothing to do with the original problem". Med Hypotheses. 67 (3): 517–23. doi:10.1016/j.mehy.2006.03.009. PMID 16632226.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) خطأ استشهاد: وسم<ref>غير صالح؛ الاسم "Moncrieff-2006" معرف أكثر من مرة بمحتويات مختلفة. - ^ Glazer, WM. (2000). "Expected incidence of tardive dyskinesia associated with atypical antipsychotics". J Clin Psychiatry. 61 Suppl 4: 21–6. PMID 10739327.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Samaha A-N, Seeman P, Stewart J, Rajabi H, Kapur S (2007). ""Breakthrough" Dopamine Supersensitivity during Ongoing Antipsychotic Treatment Leads to Treatment Failure over Time". The Journal of Neuroscience. 27 (11): 2979–2986. doi:10.1523/JNEUROSCI.5416-06.2007.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Clinical Outcome Following Neuroleptic Discontinuation in Patients With Remitted Recent-Onset Schizophrenia
- ^ Lambert, TJ. (2007). "Switching antipsychotic therapy: what to expect and clinical strategies for improving therapeutic outcomes". J Clin Psychiatry. 68 Suppl 6: 10–3. PMID 17650054.
{{cite journal}}: Cite has empty unknown parameter:|month=(help) - ^ Group, BMJ, ed. (2009). "4.2.1". British National Formulary (57 ed.). United Kingdom: Royal Pharmaceutical Society of Great Britain. p. 192. ISBN 0260-535X.
Withdrawal of antipsychotic drugs after long-term therapy should always be gradual and closely monitored to avoid the risk of acute withdrawal syndromes or rapid relapse.
{{cite book}}: Check|isbn=value: length (help); Unknown parameter|month=ignored (help) - ^ American Psychiatric Association (2004) Practice Guideline for the Treatment of Patients With Schizophrenia. Second Edition.
- ^ The Royal College of Psychiatrists & The British Psychological Society (2003). Schizophrenia. Full national clinical guideline on core interventions in primary and secondary care (PDF). London: Gaskell and the British Psychological Society.
- ^ How effective are second-generation antipsychotic drugs? A meta-analysis of placebo-controlled trials (2009)
- ^ Risperidone versus placebo for schizophrenia. Cochrane Database of Systematic (2010)
- ^ Cipriani A, Rendell JM, Geddes J (2009). "Olanzapine in long-term treatment for bipolar disorder". Cochrane Database of Systematic Reviews (Online) (1): CD004367. doi:10.1002/14651858.CD004367.pub2. PMID 19160237.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Patrick V, Levin E, Schleifer S (2005). "Antipsychotic polypharmacy: is there evidence for its use?". Journal of Psychiatric Practice. 11 (4): 248–57. doi:10.1097/00131746-200507000-00005. PMID 16041235.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Ito H, Koyama A, Higuchi T (2005). "Polypharmacy and excessive dosing: psychiatrists' perceptions of antipsychotic drug prescription". The British Journal of Psychiatry. 187: 243–7. doi:10.1192/bjp.187.3.243. PMID 16135861.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Evidence Lacking to Support Many Off-label Uses of Atypical Antipsychotics (2007)
- ^ James, A.C. (2010). "Prescribing antipsychotics for children and adolescents". Advances in Psychiatric Treatment. 16: 63. doi:10.1192/apt.bp.108.005652.
- ^ Romeo R, Knapp M, Tyrer P, Crawford M, Oliver-Africano P (2009). "The treatment of challenging behaviour in intellectual disabilities: cost-effectiveness analysis". Journal of Intellectual Disability Research. 53 (7): 633–43. doi:10.1111/j.1365-2788.2009.01180.x. PMID 19460067.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Atypical antipsychotics for aggression and psychosis in Alzheimer's disease (2006)
- ^ Jablensky A, Sartorius N, Ernberg G, Anker M, Korten A, Cooper J, Day R, Bertelsen A (1992). "Schizophrenia: manifestations, incidence and course in different cultures. A World Health Organization ten-country study". Psychol Med Monogr Suppl. 20: 1–97. doi:10.1017/S0264180100000904. PMID 1565705.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Hopper K, Wanderling J (2000). "Revisiting the developed versus developing country distinction in course and outcome in schizophrenia: results from ISoS, the WHO collaborative followup project. International Study of Schizophrenia". Schizophrenia Bulletin. 26 (4): 835–46. PMID 11087016.
- ^ Moncrieff J (2006). "Does antipsychotic withdrawal provoke psychosis? Review of the literature on rapid onset psychosis (supersensitivity psychosis) and withdrawal-related relapse". Acta Psychiatrica Scandinavica. 114 (1): 3–13. doi:10.1111/j.1600-0447.2006.00787.x. PMID 16774655.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Harrow M, Jobe TH (2007). "Factors involved in outcome and recovery in schizophrenia patients not on antipsychotic medications: a 15-year multifollow-up study". The Journal of Nervous and Mental Disease. 195 (5): 406–14. doi:10.1097/01.nmd.0000253783.32338.6e. PMID 17502806.
{{cite journal}}: Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help) - ^ Whitaker R (2004). "The case against antipsychotic drugs: a 50-year record of doing more harm than good". Medical Hypotheses. 62 (1): 5–13. doi:10.1016/S0306-9877(03)00293-7. PMID 14728997.
- ^ Myth of the antipsychotic (2008)
- ^ Methodological Issues in Current Antipsychotic Drug Trials (2008)
- ^ Geddes J, Freemantle N, Harrison P, Bebbington P (2000). "Atypical antipsychotics in the treatment of schizophrenia: systematic overview and meta-regression analysis". BMJ. 321 (7273): 1371–6. doi:10.1136/bmj.321.7273.1371. PMC 27538. PMID 11099280.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Leucht S, Wahlbeck K, Hamann J, Kissling W (2003). "New generation antipsychotics versus low-potency conventional antipsychotics: a systematic review and meta-analysis". Lancet. 361 (9369): 1581–9. doi:10.1016/S0140-6736(03)13306-5. PMID 12747876.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Davis JM, Chen N, Glick ID (2003). "A meta-analysis of the efficacy of second-generation antipsychotics". Archives of General Psychiatry. 60 (6): 553–64. doi:10.1001/archpsyc.60.6.553. PMID 12796218.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Tuunainen A, Wahlbeck K, Gilbody SM (2000). "Newer atypical antipsychotic medication versus clozapine for schizophrenia". Cochrane Database of Systematic Reviews (2): CD000966. doi:10.1002/14651858.CD000966. PMID 10796559.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ^ Ghaemi SN, Hsu DJ, Rosenquist KJ, Pardo TB, Goodwin FK (2006). "Extrapyramidal side effects with atypical neuroleptics in bipolar disorder". Progress in Neuro-psychopharmacology & Biological Psychiatry. 30 (2): 209–13. doi:10.1016/j.pnpbp.2005.10.014. PMID 16412546.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Lieberman JA, Stroup TS, McEvoy JP; et al. (2005). "Effectiveness of antipsychotic drugs in patients with chronic schizophrenia". The New England Journal of Medicine. 353 (12): 1209–23. doi:10.1056/NEJMoa051688. PMID 16172203.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Stroup T; Lieberman, JA; McEvoy, JP; Swartz, MS; Davis, SM; Rosenheck, RA; Perkins, DO; Keefe, RS; Davis, CE (2006). "Effectiveness of olanzapine, quetiapine, risperidone, and ziprasidone in patients with chronic schizophrenia following discontinuation of a previous atypical antipsychotic". Am J Psychiatry. 163 (4): 611–22. doi:10.1176/appi.ajp.163.4.611. PMID 16585435.
- ^ McEvoy J; Lieberman, JA; Stroup, TS; Davis, SM; Meltzer, HY; Rosenheck, RA; Swartz, MS; Perkins, DO; Keefe, RS (2006). "Effectiveness of clozapine versus olanzapine, quetiapine, and risperidone in patients with chronic schizophrenia that did not respond to prior atypical antipsychotic treatment". Am J Psychiatry. 163 (4): 600–10. doi:10.1176/appi.ajp.163.4.600. PMID 16585434.
- ^ Voruganti LP, Baker LK, Awad AG (2008). "New generation antipsychotic drugs and compliance behaviour". Current Opinion in Psychiatry. 21 (2): 133–9. doi:10.1097/YCO.0b013e3282f52851. PMID 18332660.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ How CATIE brought us back to Kansas: a critical re-evaluation of the concept of atypical antipsychotics and their place in the treatment of schizophrenia (2008)
- ^ Typical and Atypical Antipsychotics - The Misleading Dichotomy (2008)
- ^ Biases in Medication Prescribing: The Case of Second-Generation Antipsychotics (2010)
- ^ Swainston Harrison T, Perry CM (2004). "Aripiprazole: a review of its use in schizophrenia and schizoaffective disorder". Drugs. 64 (15): 1715–36. PMID 15257633.
- ^ Consumer Health Resource Group, LLC (2009-09-19). "Abilify Side Effects". www.askapatient.com. Retrieved 2009-09-29.
- ^ Zuardi AW, Crippa JA, Hallak JE, Moreira FA, Guimarães FS (2006). "Cannabidiol, a Cannabis sativa constituent, as an antipsychotic drug". Brazilian Journal of Medical and Biological Research. 39 (4): 421–9. doi:/S0100-879X2006000400001. PMID 16612464.
{{cite journal}}: Check|doi=value (help); Unknown parameter|doi_brokendate=ignored (|doi-broken-date=suggested) (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ أ ب Leweke, F.M.; Koethe, D.; Pahlisch, F.; Schreiber, D.; Gerth, C.W.; Nolden, B.M.; Klosterkötter, J.; Hellmich, M.; Piomelli, D. (2009). "S39-02 Antipsychotic effects of cannabidiol". European Psychiatry. 24: S207. doi:10.1016/S0924-9338(09)70440-7.
- ^ Benneyworth MA, Xiang Z, Smith RL, Garcia EE, Conn PJ, Sanders-Bush E (2007). "A selective positive allosteric modulator of metabotropic glutamate receptor subtype 2 blocks a hallucinogenic drug model of psychosis". Molecular Pharmacology. 72 (2): 477–84. doi:10.1124/mol.107.035170. PMID 17526600.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Fell MJ, Svensson KA, Johnson BG, Schoepp DD (2008). "Evidence for the role of metabotropic glutamate (mGlu)2 not mGlu3 receptors in the preclinical antipsychotic pharmacology of the mGlu2/3 receptor agonist (-)-(1R,4S,5S,6S)-4-amino-2-sulfonylbicyclo[3.1.0]hexane-4,6-dicarboxylic acid (LY404039)". The Journal of Pharmacology and Experimental Therapeutics. 326 (1): 209–17. doi:10.1124/jpet.108.136861. PMID 18424625.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ González-Maeso J, Ang RL, Yuen T; et al. (2008). "Identification of a serotonin/glutamate receptor complex implicated in psychosis". Nature. 452 (7183): 93–7. doi:10.1038/nature06612. PMC 2743172. PMID 18297054.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Patil ST, Zhang L, Martenyi F; et al. (2007). "Activation of mGlu2/3 receptors as a new approach to treat schizophrenia: a randomized Phase 2 clinical trial". Nature Medicine. 13 (9): 1102–7. doi:10.1038/nm1632. PMID 17767166.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|laydate=ignored (help); Unknown parameter|laysource=ignored (help); Unknown parameter|laysummary=ignored (help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Murphy BP, Chung YC, Park TW, McGorry PD (2006). "Pharmacological treatment of primary negative symptoms in schizophrenia: a systematic review". Schizophrenia Research. 88 (1–3): 5–25. doi:10.1016/j.schres.2006.07.002. PMID 16930948.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Vita A, De Peri L (2007). "The effects of antipsychotic treatment on cerebral structure and function in schizophrenia". International Review of Psychiatry. 19 (4): 429–36. doi:10.1080/09540260701486332. PMID 17671875.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Bonelli RM, Hofmann P, Aschoff A; et al. (2005). "The influence of psychotropic drugs on cerebral cell death: female neurovulnerability to antipsychotics". International Clinical Psychopharmacology. 20 (3): 145–9. doi:10.1097/00004850-200505000-00004. PMID 15812264.
{{cite journal}}: Explicit use of et al. in:|author=(help); Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Dorph-Petersen KA, Pierri JN, Perel JM, Sun Z, Sampson AR, Lewis DA (2005). "The influence of chronic exposure to antipsychotic medications on brain size before and after tissue fixation: a comparison of haloperidol and olanzapine in macaque monkeys". Neuropsychopharmacology. 30 (9): 1649–61. doi:10.1038/sj.npp.1300710. PMID 15756305.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Konopaske GT, Dorph-Petersen KA, Pierri JN, Wu Q, Sampson AR, Lewis DA (2007). "Effect of chronic exposure to antipsychotic medication on cell numbers in the parietal cortex of macaque monkeys". Neuropsychopharmacology. 32 (6): 1216–23. doi:10.1038/sj.npp.1301233. PMID 17063154.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ Konopaske GT, Dorph-Petersen KA, Sweet RA, Pierri JN, Zhang W, Sampson AR, Lewis DA (2008). "Effect of chronic antipsychotic exposure on astrocyte and oligodendrocyte numbers in macaque monkeys". Biol. Psychiatry. 63 (8): 759–65. doi:10.1016/j.biopsych.2007.08.018. PMC 2386415. PMID 17945195.
{{cite journal}}: Unknown parameter|month=ignored (help)CS1 maint: multiple names: authors list (link) - ^ DeLisi LE (2008). "The concept of progressive brain change in schizophrenia: implications for understanding schizophrenia". Schizophrenia Bulletin. 34 (2): 312–21. doi:10.1093/schbul/sbm164. PMC 2632405. PMID 18263882.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ GPs under 'pressure' to issue neuroleptics, claims professor, Chemist + Druggist, 15 January 2009
- ^ NEWS.BBC.co.uk
- ^ Reuters.com
- ^ Hilzenrath, David S. (January 16, 2010). "Justice suit accuses Johnson & Johnson of paying kickbacks". The Washington Post. Retrieved January 17, 2010.
- ^ أ ب Jobe TH, Harrow M (2005). "Long-term outcome of patients with schizophrenia: a review" (PDF). Canadian Journal of Psychiatry. 50 (14): 892–900. PMID 16494258. Retrieved 2008-07-05.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Kane, JM.; Leucht, S. (2008). "Unanswered questions in schizophrenia clinical trials". Schizophr Bull. 34 (2): 302–9. doi:10.1093/schbul/sbm143. PMID 18199633.
{{cite journal}}: Unknown parameter|month=ignored (help) - ^ Drug Maker’s E-Mail Released in Seroquel Lawsuit
- ^ Pharmaceutical Industry Agenda Setting in Mental Health Policies
وصلات خارجية
- Are atypical antipsychotics advantageous? - the case for, Australian Prescriber 2005 (note: pharmaceutical company conflict of interest statement at the end)
- Are atypical antipsychotics advantageous? - the case against, Australian Prescriber 2005
- Bipolar Meds - The Antipsychotics, mcmanweb.com
- FDA Public Health Advisory - Public Health Advisory for Antipsychotic Drugs used for Treatment of Behavioral Disorders in Elderly Patients, fda.gov
- FROTA LH. Partial Agonists in the Schizophrenia Armamentarium. Tardive Dysphrenia: The newest challenge to the last generation atypical antipsychotics drugs? J Bras Psiquiatr 2003; Vol 52 Supl 1;14-24. Free full-text in Portuguese with Abstracts in English, medicina.ufrj.br
- Antipsychotic Medication - information from mental health charity The Royal College of Psychiatrists
- (البرتغالية) FROTA LH. Fifty Years of Antipsychotic Drugs in Psychiatry. "Cinqüenta Anos de Medicamentos Antipsicóticos em Psiquiatria." 1st ed; Ebook: CD-Rom/On-Line Portuguese, ISBN 85-903827-1-0, File .pdf (Adobe Acrobat) 6Mb, Informática, Rio de Janeiro, august 2003, 486pp., medicina.ufrj.br
- CS1 errors: unsupported parameter
- CS1 errors: generic name
- مقالات بالمعرفة بحاجة لذكر رقم الصفحة بالمصدر
- CS1 errors: ISBN
- CS1 errors: DOI
- Articles containing إنگليزية-language text
- Pages using Lang-xx templates
- Articles containing Greek-language text
- Articles with unsourced statements from February 2009
- Articles with hatnote templates targeting a nonexistent page
- Articles with unsourced statements from April 2009
- مضادات الذهان
- ذهان
- أدوية الجهاز العصبي المركزي